
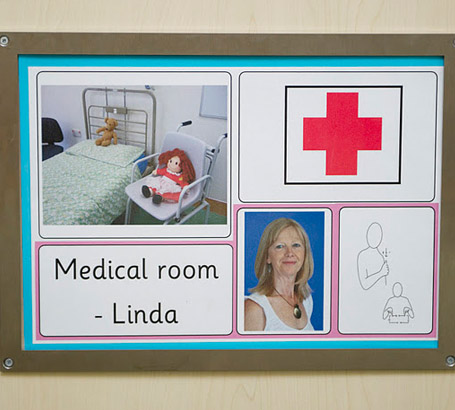
Many children and young people with SLD/PMLD/CLDD have additional medical problems needing medication and medical procedures in school. School leadership teams are responsible for drawing up individual health support procedures with medical professionals. Children and young people will have specific individual health care plans developed though discussion with school staff, the school nurse and parents.
Schools are not legally bound to administer medication, but most do so by written agreement with medical/health personnel and parents. The headteacher usually delegates this to a named person(s).
All schools will have policies, guidelines and protocols relating to the safe administration of medication. Practitioners must ensure that they follow these protocols.

Before administering medication or medical procedures to any individual, named member(s) of school staff must receive formal specialist training (generic and individual-specific) delivered by an accredited specialist health professional.
With continuing medical/health advice and support, this will enable them to carry out specific tasks in line with their school's relevant policies and guidance, and individual protocols. They must administer only prescribed and labelled medication/medical procedures with written permission from medical/health personnel, headteacher and parents. (Contingency arrangements are necessary.)
Children and young people may experience allergies, common illnesses and ailments. Household medication should only be given with written permission from medical personnel and parents.
There are specific health procedures that are not permitted to be performed by staff who are not appropriately trained nurses.
The Royal College of Nursing maintain a record of these procedures in 'Managing children with health care needs: delegation of clinical procedures, training and accountability issues' (see www.rcn.org.uk for the most recent issue).

Children with profound and multiple needs may be particularly frail and unable to withstand common illnesses.
All staff should be aware of emergency actions and protocols relating to specific individuals (eg allergic responses, epilepsy, severe asthma).
It is essential that all relevant staff are clear about how an individual's health needs will be managed at school and in what circumstances the child or young person is too unwell to attend.
If in any doubt about the medical welfare of a child or young person, school staff should be confident to call an ambulance for paramedic support.

Chemical restraint is the use of medication for the purpose
of alleviating or managing the symptoms or behaviours associated with an underlying psychological condition.
Inappropriate use of any form of restrictive physical intervention or restraint can constitute assault or negligence. This
is also true of chemical restraint where its use is not appropriate.
British Institute of Learning Disabilities, 2008

It is essential to have a written health care plan for
each child or young person who requires invasive treatment or clinical procedures. The plan should include instructions on
the specific procedure and information for dealing with an emergency situation. The plan must be drawn up in conjunction with
a health care professional and approved by a doctor or a nurse from the Children's Community Nursing Service or School Health
Service. The health care plan should be reviewed and updated annually [or more often if necessary].
Lenehan, 2004

British Institute of Learning Difficulties (2008) Factsheet: Chemical Restraint.
Cope, P. / Children and Young People's Services, Milton Keynes Council (2010) Children and young people with medical and physical difficulties: Information for schools, early years and other community settings. Milton Keynes: Milton Keynes Council.
Department for Education and Skills / Department of Health (2005, updated 2007), Managing Medicines in Schools and Early Years Settings.
Lenehan, C., Morrison, J. and Stanley, J. (2004) The Dignity of Risk: A practical handbook for professionals working
with disabled children and their families. London: Council for
Disabled Children/Shared Care.

Matousova-Done, Z. and Gates, B. (2006) The nature of care planning and delivery in intellectual disability nursing. In: B. Gates (ed.) Care Planning and Delivery in Intellectual Disability Nursing. Oxford: Blackwell.
Mencap (2010) Understanding profound and multiple learning disabilities (Appendix 1 of Written evidence submitted by Mencap. In: Education Committee (2011) Education: Third report. London: House of Commons.

Postural Care Action Group (2011) Postural care. For the video, booklet and presentation, visit http://www.mencap.org.uk/posturalcare.
Royal College of Nursing (2008) Managing Children with Health Care Needs: Delegation of clinical procedures, training and accountability issues. London: Royal College of Nursing.
Medical Conditions at School Partnership (2007)Medical Conditions at School Policy Pack & Forms.
Turner, P. (2007) Your responsibility for administering medicines, Primary Headship.