
It is important that each child or young person with SLD/PMLD/CLDD is able to achieve the best possible health they can. All children with complex health needs will have a paediatrician whose specific role is to co-ordinate and manage medical needs, referrals to specialists etc. The role of the school is to ensure good communication with the consultant paediatrician so that there is good two-way information on a regular basis and a shared approach. The school nurse is key in this.
Complex health conditions may include:
- Complex epilepsy.
- Technological dependency (eg needing oxygen, tube feeding or suctioning equipment).
- 'Life-limiting' conditions.
- Fragile health, leading to increased risk of chest infections and gastro-intestinal conditions.
(Mencap, 2010)

To safeguard children and young people, the responsibilities of a headteacher include ensuring that:
- Appropriate medical information about a child or young person is shared with staff on a 'need to know' basis.
- Routine and contingency protocols around medication are established, and the necessary consents are obtained.
- Appropriate staff are contracted to carry out the medical/health/personal care tasks needed.
- There are appropriate facilities to carry out the tasks.
- Identifying staff to administer medication and medical procedures (see Level C for more details).
- Staff receive appropriate training.

The responsibilities of staff include:
- Clear communication with parents over the daily care of children with medical needs.
- Being familiar with the contents of a child or young person's health care plan.
- Knowing and being confident of carrying out medical protocols for the young people in their care (routine and contingency).
- Taking the child or young person's medical requirements into consideration in any activity.
- Implementing the protocols, and taking all reasonable steps to avoid disruption.
- If disruption is unavoidable, knowing what course of action to take.

Children and young people with mobility difficulties may use a wheelchair, and be unable to control or vary their posture efficiently.
These individuals will need specialised equipment to aid their mobility, to support their posture and to protect and restore their body shape, muscle tone and quality of life.
It is vital that people with physical needs have access to physiotherapy, occupational therapy and hydrotherapy, and that their carers receive training to enable them to manage their physical needs confidently on a day-to-day basis.
(Mencap, 2010)
 0
0
Children and young people with SLD/PMLD/CLDD may not be able to understand or communicate pain associated with their condition or other common ailments (eg toothache). It is important to be aware of signs of discomfort or unease (eg unexplained changes in behaviour).
Read Cunningham (2010) to see the difference that appropriate management of medical difficulties made for one young person.
Think of a young person you know with complex medical needs. Work with others who know them well to catalogue their physical signs of discomfort, and how to respond to them.

- Intimate care policy.
- Infection control policy.
- Moving and handling policy.
- Safeguarding policy.
- Health and safety policy.
- Administration of medication.
- First aid policy.
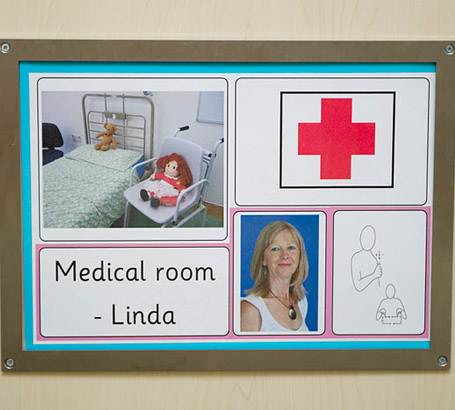
- School nurse.
- Respiratory nurse.
- Occupational therapist.
- Community learning disabilities team.
- Paediatric consultant.
- Paediatric nursing service.
