
The resources at this level provide an insight into the diagnosis and identification of mental health.
Some key issues in this area are explored.

Diagnosis is commonly used by medical professionals to identify and label the problem or difficulty as it is perceived by one or more professionals.
Where behaviours or symptoms cluster together, classification systems are used to diagnose or determine what the difficulty is.

From a clinical perspective it allows professionals to develop a specific intervention plan to treat the condition or illness.
Mental health difficulties can also be 'diagnosed' and correct diagnosis should lead to appropriate intervention.

Clinical professionals recognise there are inherent difficulties in detecting mental health problems in persons with SLD/PMLD/CLDD due to:
- The need for further staff training;
- Over reliance on teachers and schools ability to recognise and report symptoms of ill health;
- Usually requiring the client to have good linguistic abilities;
- Different presentations and behaviours in persons with SLD/PMLD/CLDD.
From an educational perspective there will sometimes be a case for a more ecological or systemic perspective and hypotheses that can be tested should be used – and sometimes changed if the evidence from sustained observation or intervention does not support them.

Diagnosing mental health difficulties in this group of the population is a complex and difficult task.
The difficulties are mainly due to lack of consensus as to which instruments are sufficiently valid and reliable for the screening and diagnosis of such disorders in people with learning difficulties. But also the client might have difficulty in communicating effectively his or her internal thoughts and mental state.

The term 'diagnostic overshadowing' (Smiley and Cooper, 2003) increased awareness of the diagnostic challenges that clinicians encounter in attempting to diagnose psychological and emotional problems in people with learning difficulties.
The importance of present classification systems being developmentally appropriate has been emphasised (Cooper et al, 2003).
The inability to communicate accurately the more abstract aspects of mental state may render inappropriate the use of standard methods of diagnosis for the general population (Sturmey et al, 1991).
More recently, an effort has been made to establish diagnostic criteria to provide different 'gold standards' for a given psychiatric disorder depending on the level of learning difficulty.
There is often a tendency to make sense of unusual or bizarre behaviours, purely from a behavioural perspective or framework.
- Attention seeking
- Boldness
- Cheekiness
As practitioners and educators, we need to challenge these assumptions and examine other possible frameworks for investigating.
Unusual behaviours may be observed, but there may be an underlying mental health component to the young person's presentation (Coughlan, 2010).
There might also be systemic and ecological reasons that need to be examined. Identifying the reasons for presenting behaviours is a complex and time consuming process if it is to be done well. This is especially the case with those clients who also have learning difficulties.
A multi-professional approach will often be required.

Undertake a comprehensive assessment by:
- Building up a picture of the persons behaviour – signs, symptoms, contextual factors;
- Developing a number of hypotheses to
be tested; - Referring to the diagnostic criteria – do the symptoms match the criteria?;
- Taking a team approach – as the entire team should be seen as 'clinical
information gatherers'.
assessment policy

Ask yourself the following key questions:
- What signs, symptoms and environmental factors do you take into consideration in your in relation to your school and classroom?
- How does your assessment policy ensure that complex needs are accurately identified and that behaviours are not misinterpreted with the risk of mental health difficulties going undetected?
- What impact does this have on the outcomes of young people?

Read the following case study on Brian and answer the questions at the foot of the document.
Many of the questions are for members of the multidisciplinary team – however, teachers are an essential part of this team.
Discuss the role of the teacher in this process with your colleagues.
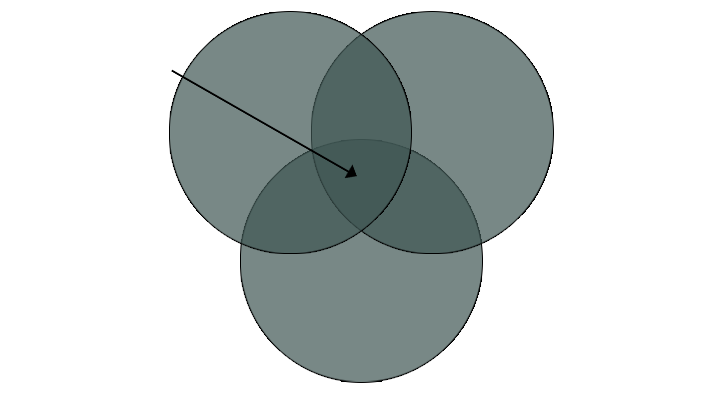
High Risk
Biological
Developmental
Psychological
Social
Different genetic syndromes, Impariment of brain function, Physical Illnesses, Susceptibility to mental illness, Severe
and complex epilepsy, Sensory and
physical impairments
Psychological, sexual and physical abuse, Lack of meaningful oportunities, Negative life experiences, No engagement in
day to day activities, Denial of individual needs, Atmosphere of blame, High levels of cerer stress, Gender, race, ethnic
and
other discrimination
Cognitive strengths and weaknesses, Other neuropsychological impairments, Reinforcement of maladaptive behaviours, Impaired language development, Poor self-esteem, Peceived lack of emotional support, Impact of adverse life events

Cooper, S.A., Smiley, E., Finlayson, J., Jackson, A., Allan, L., Williamson, A., Mantry, D. & Morrison, J. (2007) The Prevalence, Incidence and Factors Predictive of Mental Ill-Health in Adults with Profound Intellectual Disabilities. Journal of Applied Research in Intellectual Disabilities, 20, 493-501.
Smiley, E, and Cooper, SA (2003) Intellectual disabilities, depressive episode, diagnostic criteria and Diagnostic Criteria for Psychiatric Disorders for Use with Adults with Learning Disabilities/Mental Retardation (DC-LD). Journal of Intellectual Disability Research, 47 (Suppl.). pp. 62-71.
Sturmey, P.,Reed,J.&Corbett, J.(1991) Psychometric assessment of Psychiatric disorders in people with learning difficulties (mental handicap): a review of measures. Psychological Medicine, 21, 143-155.